Amitriptyline the medication to consider for lumbar spinal stenosis with sciatica
As an experienced physiotherapist working in primary care, my caseload hosts some of the oldest patients in the UK. The patient at the centre of this case study is ‘Mrs G’ who was referred to me via her GP for back and leg pain, a condition I treated with amitriptyline.
Mrs G is a 75-year-old retired administrator with a long history of mild episodic back pain, typically, her pain is self-managed with exercises and occasional paracetamol, she does not take any other medication. Ten weeks ago, she was gardening and her back became stiff, she sat and rested for the evening. The next day saw the onset of right leg pain and paresthesia in her lateral foot, she scores the pain on the visual analogue scale 7/10 upon walking 100 yards. Ambulatory symptoms are eased with sitting or pushing her shopping trolley. Symptoms gradually worsened over the coming weeks, and she experienced night cramps and disturbed sleep, her usual methods of self-management were no longer effective. She reported this to her GP at a recent health check and received a referral to physiotherapy and a blood test which showed good renal function and no abnormal inflammatory or tumor markers. There were no red flags, allergies, intolerances or family history of inflammatory disease and her past medical history was void of any comorbidities, she was otherwise fit and well.
What takes place within the assessment
An MSK practitioner’s assessment follows a well-established process of deductive reasoning (Petty and Moore, 2001). Mrs G presented with a slightly flexed lumbar posture and she walked in this position as it was more comfortable, her back was stiff and limited in a capsular pattern of discomfort, suggestive of either degenerative changes or an acute inflammatory component (Atkins et al., 2010). Her neurological assessment was abnormal and showed reduced right L5 and S1 dermatomes, a minimal reduction in S1 myotome (plantar flexion) but normal reflexes including Babinski. The specificity of these tests are regularly debated in the literature, but general consensus offers a spinal neural component to her pain at perhaps more than one level, but leads diagnosis away from an upper motor neuron lesion i.e stroke (Petty and Ryder, 2017). More support is offered with a sciatic straight leg raise of 75/65 degrees of movement, this is mildly positive for her leg pain and implicates the sciatic nerve (Butler, 1991). There was local tenderness at L5 vertebra on passive accessory mobilization, this offers a site for pathology (Maitland et al., 2005). There was no pain on percussions. The patient had normal symmetrical foot pulses suggesting good, equal vascular leg circulation and the absence of true claudication (Camm, 2009).
What else could cause back and leg pain
In a patient of this age the differential diagnoses could be fracture, perhaps from excessive forces whilst gardening, paying toll on osteoporotic vertebra. As there was no history of trauma, manual percussions were not painful, and no history of fractures identifying unsatisfactory bone density, that diagnosis seems unlikely (Atkins et al., 2010). As was a pathological fracture from chondrosarcoma, which is rare, typically only 550 patients are diagnosed annually in the UK and patients become very unwell (NHS choices, 2018). Sometimes tumours markers can be picked up on blood tests, but no issues were highlighted for further investigation (Greenhalgh et al., 2006).
What is lumbar spinal stenosis
Spinal stenosis is described as a medical condition in which the spinal canal narrows as a person ages and compresses or irritates the spinal cord or nerves descending there from, at the level of the lumbar vertebra (Zhou et al., 2017). There is surgical evidence that suggests patients with severe resistive symptoms have an anatomical predisposition to foraminal stenosis, namely a larger pedicle height to vertebral body height ratio, leaving less room below the pedicle for the exiting nerve root compared to asymptomatic patients (Merckaert et al, 2015). The term spinal stenosis does not appear to be specific to one pathoanatomical finding, it can have a degenerative inflammatory component and or a mechanical neural interface as seen in vertebral spondylolisthesis, facet joint hyperplasia, bony spur posterior extension, intervertebral disc prolapse/protrusion, and ligamentum flavum hypertrophy (Zhou et al., 2017).
Anatomy and treatment video by Nuvasive.com

How do I know its lumbar spinal stenosis
Tomkins-Lane et al (2016) delivered an online survey to 279 clinicians from the international society for the study of the lumbar spine, and asked specialists to express in logical order which assessment findings they most commonly expect in this diagnosis. In the appendix you can find seven questions which the research offers as a tool that can; with 80% (P<.05) certainty, clinically diagnose lumbar spinal stenosis. Mrs G presents with all seven markers.
- Does the patient have leg or buttock pain while walking?
- Does the patient flex forward to relieve symptoms?
- Does the patient feel relief when using a shopping cart or bicycle?
- Does the patient have motor or sensory disturbance while walking?
- Does the patient have normal and symmetric foot pulses?
- Does the patient have lower extremity weakness?
- Does the patient have Low back pain?
How common is spinal stenosis
The prevalence of lumbar spinal stenosis is approximately 9.3% in developed western populations, with people most commonly affected in the sixth or seventh decade of life (Schroeder et al., 2016). It appears to be a global health problem, it has no cure, the conditions physical and personal effects threaten efforts to support healthy ageing (Ferreira and de Luca, 2017). Patients often have pain, cramping, and weakness in their legs that is worsened with standing and walking (Schroeder et al., 2016). Treatments include physiotherapy; manual therapy and exercises, caudal epidural, or non-steroidal anti-inflammatory drugs in renally healthy populations (Aichmair et al., 2017; BNF, 2016). I suspect Mrs G’s condition is approaching a more severe end-stage, where the burden of spinal pain has a considerable impact on her wellbeing and independence (Ferreira and de Luca, 2017).
What are the frontline medications
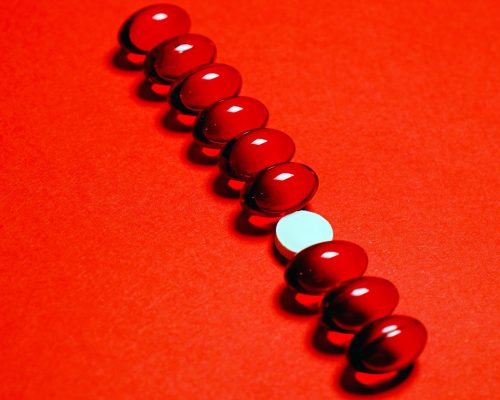
Tricyclic anti-depressants are recommended for use in the NICE low back pain guidance (2009), and again the NICE guidance for neuropathic pain (updated 2017) which stipulates amitriptyline, as initial front line pharmacological treatment. Amitriptyline is licensed as an antidepressant and for nocturnal enuresis and not for pain relief so in this instance it will be prescribed ‘off label’, adding a layer of legal accountability (Dawson et al., 2014).
The pharmocokinetics of amitriptyline
The drug was synthesized in 1949 as a potential anti-psychotic drug and it is related to phenothiazines. It is a tertiary amine with two methyl groups attached to the basic nitrogen atom (Ryu et al., 2017) .
It is freely soluble in water, and absorbed through the intestine, it is dispensed in boxes of 28, with oral administration of tablets sized 10mg, 25mg or 50mg. Maximum serum levels are achieved in about 4 hours and steady state reached in a week, plasma protein binding is about 95% with bioavailability at 53% (EMC, 2018).
Absorbtion
Amitriptyline is rapidly demethylated into secondary amines such as nortriptyline with immediate effects compete for the binding sites on neurons, blocking the reuptake of amines by the nerve terminal. They have strong serotoninergic and noradrenergic reuptake inhibition with additional sodium and calcium channel blockade activity (Sawynok et al., 2001). This accounts for the improved emotional symptoms, whereas relief of biological symptoms results from facilitation of noradrenergic transmission effectively raising the threshold of neural firing and dampening neuropathic symptoms, a most desirable outcome (Rang and Dale’s, 2007).
Distribution
The metabolism of amitriptyline proceeds mainly by demethylation (CYP2C19, CYP3A4) and hydroxylation (CYP2D6) followed by conjugation with glucuronic acid (Rang and Dale’s, 2007). Pharmacokinetic properties highlighted by a new US government trial (2018) offer the metabolism of amitriptyline by CYP2D6 and CYP2D19 isoenzymes found in the intestine and liver. These are highly polymorphic in nature with numerous genetic variants, this offers a possible explanation as to why only one in three patients are responders to amitriptyline. In contrast to this, Ryu et al (2017) performed a genotype stratification study on 24 healthy Koreans, taking blood samples after 25mg of Amitriptyline. They offer that the metabolic pathway was more dominant by CYP2C19 than CYP2D6 and that gene variations did not change the pharmacodynamic effect. This opens the possibility of severe adverse effects arising from ‘poor metabolisers’ deficient in the enzyme CYP2C19, thus hepatic impairment may reduce extraction resulting in higher plasma levels and caution should be exercised when dosing these patients (EMC, 2018).
Metabolism
The drug is excreted renally, elimination half-life (t½ β) of amitriptyline is about 25 hours in healthy test populations (24.65±6.31 hours; range 16.49-40.36 hours) and mean systemic clearance (healthy 39.24±10.18 L/h, range 24.53-53.73 L/h). It is estimated that people over 70 have 50% reduced renal function and demonstrate longer half-lives (EMC, 2018; Rang and Dale’s, 2007). This influences plasma concentrations, causes side effects and impacts negatively on concordance, which is why follow up appointments are recommended to monitor effects (BNF, 2016).
Excretion
Why is amitriptyline not prescribed for back pain alone
Staiger et al (2003) performed a comprehensive systematic review of randomized, placebo-controlled trials of patients with acute or chronic back pain treated with various classes of oral antidepressant. They used a modified version of the reputable Cochrane Back Review Group quality scale, but controversially they did not specify if they had validated this tool. They identified 22 drug trials and excluded 15 for methodological flaws, 9 for lacking placebo groups, and 2 for including patients with neck pain. Of the remaining seven trials, their heterogeneity of their design meant a pooled estimate of effect was not possible. Despite the resulting synthesis of evidence concluding that tricyclic anti-depressants (TCA’s) are moderately effective in reducing pain, and selective serotonin reuptake inhibitors (SSRIs) were not, they importantly accepted that more research of better quality was needed in the area of back pain.
What is the evidence in support of amitriptyline off label
A more recent publication by the Special Interest Group on Neuropathic Pain (Finnerup et al., 2015) provided an update of evidence-based recommendations for pharmacological treatment. It used a different assessment method than Staiger et al (2003), through grading of recommendations assessment, development, and evaluation (GRADE), and its methodology went one step further by including a meta-analysis of vastly more studies (n=229). The primary measure was number needed to treat (NNT) for 50% pain relief and the trial outcomes were generally modest, with results complementing Staiger (2003) conclusion indicating lower number needed to treat for TCAs compared to SSRIs, and at a lower cost. Within both reviews there is a clear lack of trials on spinal stenosis with sciatica, often trials focus on trigeminal neuralgia, peripheral neuropathy, fibromyalgia, migraines, complex regional pain syndrome or postherpetic pain. They have issues with heterogeneous data, lack placebo controls and flawed blinding strategies. Yet authors offer that best evidence supports TCAs as a first line treatment for neuropathic pain, a recommendation taken to guide the treatment low back pain and sciatica (NICE, 2016). Amitriptyline does not have a UK marketing authorisation for neuropathic pain, duloxetine was licensed for diabetic peripheral neuropathic pain only, and gabapentin was licensed for peripheral neuropathic pain only, so use for other conditions would be off-label (NICE 2013). It is conceivable that this evidence and that previously discussed on pharmacokinetic ‘poor metabolisers’ of amitriptyline, support pharmacological advice that failure with one medication in the management of neuropathic pain, does not necessarily predict failure with another, simply switch drugs (Dawson et al 2014).
Benefits of amitriptyline
One prospective randomised controlled trial compared amitriptyline, nortriptyline against combining drugs (adjuvant therapy) for peripheral neuropathy (Liu et al., 2014). There were 5 arms, the trial included a control the two drug groups and 2 adjuvant medical therapies groups for concomitant medication. The Douleur Neuropathique en 4 (DN4) questionnaire was used alongside a plethora of validated outcome measures to assess 178 patients over a 6 month period. Results show the benefits seen in the TCA groups and adjuvant therapy groups were typically VAS pain reduction estimated to be 25%, also sleep, anxiety, depression, and quality of life significantly improved in these cohorts. Although there were similar methodological flaws to papers previously critiqued (Finnerup et al., 2015; Staiger et al., 2003), this study (Liu et al., 2014) design mimicked a real world variable dosing strategy and offers the possibility to combine medication to achieve pain relief in more patients, providing support for adjuvant therapy and the advice to switch drugs when treatment fails (Dawson et al., 2014) as the next medication may metabolise successfully.
Adverse effects of amitriptyline
This trial (Liu et al., 2014) attempted to quantify its adverse events and defined them as a noxious and unintended or unexpected response, this study found none within the serious category, however there was a clear discontinuation due to adverse effects or inefficacy in 26–37% of patients receiving these TCAs. There are published cases of serious adverse effects from amitriptyline, namely were the desired outcome of a patient’s action was a deliberate overdose. With the serotonergic mechanism providing emotional relief and the sedative effect offering an escape from the pain, the author alleged it is one of the commonest causes of drug poisoning (Kansal et al, 2017). Tanaka et al (1998) provided a review of published reports showing interactions between acute ingestion of alcohol (ethanol) and tranquilizers or hypnotics, including TCAs. They highlighted the pharmacokinetic interactions within the cytochrome P450 isoenzymes that catalyse the drugs. Identifying in recent years significant clinical implications: impairment of many motor, sensory and neurological functions and, possibly sudden death. In-light of all these known harms, there will be occasions where the patients past medical history has complications such as liver failure or significant cardiac disease, under these circumstances a clinical pharmacist would provide some guidance on dosing and monitoring.

Side effects – amitriptyline
drowsiness, dizziness, postural hypotension, nausea, constipation, blurred vision, dry mouth, difficulty with micturition, sinus tachycardia, agitation, hyponatraemia, lower seizure threshold (BNF 2016)
Cautions
Epilepsy, closed angle glaucoma, liver disease, cardiac disease, thyrotoxosis, psychoses, prostatic hypertrophy or urinary retention, porphyria, (Dawson et al 2014)
Contra-indications
Acute porphyrias, arrhythmias, during manic phase of bipolar disorder, heart block, immediate recovery period after myocardial infarction. (BNF, 2016)
Consent
There is a balance between the clinical benefit of prescribing and the likelihood of adverse effects. Special efforts need to be taken to achieve informed consent (CSP, 2002; HCPC, 2011a), the Department of Health suggest informed consent is best achieved by giving patients time to reflect on information before starting treatment (DOH, 2009). A discussion about side effect and issues with concordance is recommended with provision of a clear and understandable advisory leaflet from the faculty of pain medicine (FPM, 2014). It is also good practice to grade treatment effectiveness, and in this case study there was a shared decision to adopt a pain score (VAS) and a functional outcome measure; walking distance, these are evidence based and SMART (Aicher et al., 2012; Williams et al., 2017).
Dosing changes and monitoring patients
It can be reasoned that elderly patients are more sensitive to these drugs as metabolism is less vigorous, so a shared the decision to take steps to minimise adverse effects by reducing the starting dose to 5mg is recommended (BMA, 2015). Sometimes follow up telephone appointments can be useful to appropriately monitor drug titration; week one 10mg, week two 20mg (BNF, 2016). One critical area to discuss is the sedative effects and necessary instructions to take amitriptyline 2-4 hours before planned sleep, rather than at bedtime is useful, as this helps to reduce the hangover effect in the morning (Dawson et al., 2014). It is useful to provide some perspective, offering the maximum adult dose as 75mg and to expect to be taking the medication regularly for several months because her condition was not curable (BNF, 2016; Weinstein et al., 2008).
Case outcome
By the fourth week Mrs G felt in control of her pain (VAS 4/10) and this was reflected in her ambulatory distance of half a mile, albeit with rest stops. Her side effects had reduced too, and she felt back to her previous self. We discussed the treatment cessation strategy in the BNF (2016), reducing the dose back down to 10mg over a five-day period and then over the following month to slowly stop the medication should she feel comfortable. Restarting the medication was advised if symptoms returned and continuing her exercises daily would achieve better self-management. In summary, with a confident diagnosis, useful patient information, the right patient will respond well to amitriptyline.

References
Aichmair, A., Burgstaller, J.M., Schwenkglenks, M., Steurer, J., Porchet, F., Brunner, F., Farshad, M., LSOS Study Group, 2017. Cost-effectiveness of conservative versus surgical treatment strategies of lumbar spinal stenosis in the Swiss setting: analysis of the prospective multicenter Lumbar Stenosis Outcome Study (LSOS). Eur Spine J 26, 501–509. https://doi.org/10.1007/s00586-016-4937-y
Atkins, E., Kerr, J., Goodlad, E., 2010. A Practical Approach to Orthopaedic Medicine: Assessment, Diagnosis, Treatment, 3e, 3 edition. ed. Churchill Livingstone, Edinburgh ; New York.
BNF, 2016. British National Formulary. BMJ Group, British Medical Association & Royal Pharmaceutical Society, London.
Butler, D., 1991. Mobilisation of the Nervous System, 1e, First Edition edition. ed. Churchill Livingstone, Edinburgh.
Camm, J., 2009. The ESC Textbook of Cardiovascular Medicine, 2 edition. ed. OUP Oxford, Oxford ; New York.
CSP, 2002. Rules of professional conduct. Chartered Society of Physiotherapy. [WWW Document]. URL http://www.csp.org.uk/publications/code-members-professional-values-behaviour (accessed 4.24.18).
Dawson, J., Hennell, S., Stephton, R., 2014. Practical Prescribing for Musculoskeletal Practitioners, 2nd ed. M&Kupdate.
DOH, 2009. Reference guide to consent for examination or treatment. 2nd Edition. Department of Health.
EMC, 2018. Amitriptyline 10mg Film-coated Tablets – Summary of Product Characteristics (SmPC) – (eMC) [WWW Document]. URL https://www.medicines.org.uk/emc/product/6017/smpc (accessed 4.23.18).
Ferreira, M.L., de Luca, K., 2017. Spinal pain and its impact on older people. Best Pract Res Clin Rheumatol 31, 192–202. https://doi.org/10.1016/j.berh.2017.08.006
Finnerup, N.B., Attal, N., Haroutounian, S., McNicol, E., Baron, R., Dworkin, R.H., Gilron, I., Haanpää, M., Hansson, P., Jensen, T.S., Kamerman, P.R., Lund, K., Moore, A., Raja, S.N., Rice, A.S.C., Rowbotham, M., Sena, E., Siddall, P., Smith, B.H., Wallace, M., 2015. Pharmacotherapy for neuropathic pain in adults: a systematic review and meta-analysis. The Lancet Neurology 14, 162–173. https://doi.org/10.1016/S1474-4422(14)70251-0
FPM, 2014. Information for adult patients prescribed amitriptyline for the treatment of pain. Faculty of pain medicine Version 1 June 2014.
Gov, 2012. The Human Medicines Regulations 2012 [WWW Document]. URL http://www.legislation.gov.uk/uksi/2012/1916/contents/made (accessed 4.17.18).
Greenhalgh, S., Selfe, J., Gifford, L., 2006. Red Flags: A Guide to Identifying Serious Pathology of the Spine, 1e, 1 edition. ed. Churchill Livingstone, Edinburgh.
HCPC, 2011a. Professionalism in healthcare professionals.
HCPC, 2011b. Continuing professional development and your registration. Health & Care Professions Council.
Kolb, D.A., 1983. Experiential Learning: Experience as the Source of Learning and Development, 1 edition. ed. Prentice Hall, Englewood Cliffs, N.J.
Kurtz, S., Silverman, J., Benson, J., Draper, J., 2003. Marrying Content and Process in Clinical Method Teaching: Enhancing the Calgary-Cambridge Guides. Academic Medicine, 78 (8), 802–809.
Liu, W.-Q., Kanungo, A., Toth, C., 2014. Equivalency of tricyclic antidepressants in open-label neuropathic pain study. Acta Neurol. Scand. 129, 132–141. https://doi.org/10.1111/ane.12169
Local Formulary, 2018. Dorset Formulary. Dorset NHS [WWW Document]. URL http://www.dorsetformulary.nhs.uk/chaptersSubDetails.asp?FormularySectionID=4&SubSectionRef=04.07.03&SubSectionID=A100&drugmatch=2424#2424 (accessed 4.29.18).
Maitland, G., Hengeveld, E., Banks, K., English, K., 2005. Maitland’s Vertebral Manipulation, 7e, 7 edition. ed. Butterworth-Heinemann, Edinburgh; New York.
NHS choices, 2018. Bone cancer [WWW Document]. nhs.uk. URL https://www.nhs.uk/conditions/bone-cancer/ (accessed 4.21.18).
NICE, 2016. Low back pain and sciatica in over 16s: assessment and management [WWW Document]. URL https://www.nice.org.uk/guidance/NG59/chapter/Recommendations#non-invasive-treatments-for-low-back-pain-and-sciatica (accessed 4.10.18).
Petty, Moore, 2001. Neuromusculoskeletal Examination and Assessment: A Handbook for Therapists, 2nd ed. Churchill Livingstone, Elsevier.
Petty, N., Ryder, D. (Eds.), 2017. Musculoskeletal Examination and Assessment – Volume 1: A Handbook for Therapists, 5e, 5 edition. ed. Elsevier, Edinburgh.
Rang, H., Dale’s, M., 2007. Rang & Dale’s Pharmacology, 6th ed. Churchill Livingstone, Elsevier.
RPS, 2016. Royal Pharmaceutical Society, 2016. A competency framework for all prescribers. [WWW Document]. URL https://www.rpharms.com/Portals/0/RPS%20document%20library/Open%20access/Professional%20standards/Prescribing%20competency%20framework/prescribing-competency-framework.pdf (accessed 4.10.18).
Ryu, S., Park, S., Lee, J.H., Kim, Y.R., Na, H.S., Lim, H.S., Choi, H.Y., Hwang, I.Y., Lee, J.G., Park, Z.W., Oh, W.Y., Kim, J.M., Choi, S.E., 2017. A Study on CYP2C19 and CYP2D6 Polymorphic Effects on Pharmacokinetics and Pharmacodynamics of Amitriptyline in Healthy Koreans. Clin Transl Sci 10, 93–101. https://doi.org/10.1111/cts.12451
Sawynok, J., Esser, M.J., Reid, A.R., 2001. Antidepressants as analgesics: an overview of central and peripheral mechanisms of action. J Psychiatry Neurosci 26, 21–29.
Schroeder, G.D., Kurd, M.F., Vaccaro, A.R., 2016. Lumbar Spinal Stenosis: How Is It Classified? JAAOS – Journal of the American Academy of Orthopaedic Surgeons 24, 843. https://doi.org/10.5435/JAAOS-D-15-00034
Staiger, T., Gaster, B., D Sullivan, M., Deyo, R., 2003. Systematic Review of Antidepressants in the Treatment of Chronic Low Back Pain. Spine. https://doi.org/10.1097/01.BRS.0000092372.73527.BA
Tomkins-Lane, C., Melloh, M., Lurie, J., Smuck, M., Battié, M.C., Freeman, B., Samartzis, D., Hu, R., Barz, T., Stuber, K., Schneider, M., Haig, A., Schizas, C., Cheung, J.P.Y., Mannion, A.F., Staub, L., Comer, C., Macedo, L., Ahn, S.-H., Takahashi, K., Sandella, D., 2016. ISSLS Prize Winner: Consensus on the Clinical Diagnosis of Lumbar Spinal Stenosis: Results of an International Delphi Study. Spine 41, 1239–1246. https://doi.org/10.1097/BRS.0000000000001476
Weinstein, J.N., Tosteson, T.D., Lurie, J.D., Tosteson, A.N.A., Blood, E., Hanscom, B., Herkowitz, H., Cammisa, F., Albert, T., Boden, S.D., Hilibrand, A., Goldberg, H., Berven, S., An, H., 2008. Surgical versus Nonsurgical Therapy for Lumbar Spinal Stenosis. N Engl J Med 358, 794–810. https://doi.org/10.1056/NEJMoa0707136
Zhou, G., Zhang, Y., Huang, W., 2017. Risk factors for ligamentum flavum hypertrophy in lumbar spinal stenosis patients from the Xinjiang Uygur Autonomous Region, China: protocol for a retrospective, single-center study. Clinical Trials in Orthopedic Disorders, China 2, 11–17.

